Niger J Paed 2015; 42 (1): 68 –70
CASE
REPORT
Oyenusi EE
Haemolacria (bloody tears): A
Ananti CH
perplexing symptom: A report of
two cases
DOI:http://dx.doi.org/10.4314/njp.v42i1,15
Accepted: 6th August 2014
Abstract: We
present two
cases
not recurred after being followed
of
a boy and a girl (both aged four
up
for two years.
Oyenusi EE
(
)
years) who presented with bloody
The
second patient, presented with
Department of Paediatrics,
tears. (haemolacria). The boy ini-
redness of the eyes and yellowish
Lagos University Teaching Hospital,
Idi-Araba, Lagos
tially presented with cough,
mucoid discharge of six days, low-
Email: ebikike@yahoo.com
catarrh and three episodes of epis-
grade fever of three days and spon-
taxis. Full blood count, coagula-
taneous bloody tears from both
Ananti CH
tion profile, bleeding time, blood
eyes. There was associated orbital
Motayo Hospital Limited,
film picture and X-ray of the post-
cellulitis and vomiting of non-
3
Owodunni Street, Ikeja, Lagos
nasal space were normal. He
bloody recently ingested feeds.
started shedding blood stained
Blood investigations were sugges-
tears initially on crying, two
tive of sepsis and assays of meas-
weeks later without associated
ured clotting factors and coagula-
epistaxis.
Subsequently
the
tion profile were normal. She was
bloody tearing became spontane-
managed with antibiotics and im-
ous. He was given intramuscular
proved with resolution of haemo-
vitamin K and high dose vitamin
lacria which has not recurred dur-
C.
Other relevant investigations to
ing a follow up period of six
determine the cause could not be
months.
done
due to financial constraints,
however
the
bloody
tearing
Key words: Bloody
tears, haemo-
stopped after two months and has
lacria, children.
Introduction
Case presentation
Case 1
Haemolacria (bloody tears) is a rare occurrence. This
rarity is alluded to in a local Nigerian (Ibo) proverb
TA, a four-year old boy initially presented in a private
which when translated means “there is nothing that the
hospital with cough, catarrh and three episodes of epis-
eye
sees and cries blood, it can only cry water”. How-
taxis.
There was no history of trauma, no previous
ever when haemolacria occurs, it may be a cause of
bleeding episodes nor a family history of bleeding disor-
panic for the patient or care givers and may perplex the
ders. He was placed on Otrivin ® nasal
drops, Actifed ®,
doctor.
It was first described by Dodanaeus
1
in
Cefuroxime, and a stat dose of diacynone. Full blood
1581where he recorded his observations on a girl who,
count, coagulation profile, bleeding time, blood film
at
the age of 16, had not menstruated. Haemolacria can
picture and X-ray of the postnasal space were normal.
be
caused by diseases of the conjunctiva, eyelids and
He
started shedding blood–stained tears initially on cry-
nasolacrimal
system or trauma . Epistaxis with retro-
2
ing, two weeks later without associated epistaxis. Subse-
grade flow, vascular malformations, inherited bleeding
quently the bloody tearing became spontaneous. The
disorders, acquired systemic coagulopathies, vicarious
eyes were grossly normal. Assays for Factors VIII, IX
menstruation, drugs, hyperthyroidism, nasolacrimal tu-
and Von Willebrand factor, a nasolacrimal irrigation and
berculosis, hysteria/stigmatization and malingering have
biopsy, CT Scan and/or MRI of the head and orbit were
also been implicated . Haemolacria can also be idio-
3-9
planned for but the health insurance did not cover the
pathic .
2
expenses and the parents had financial constraints. He
We
report these two cases to draw attention of clinicians
was given empirical therapy of IM Vitamin K for three
days and placed on high dose Vitamin C (500mg daily) .
6
to
this unusual condition and highlight management
challenges.
Two months later, the bloody tearing stopped spontane-
ously and he has been stable for about 18 months.
69
Case 2
girl with an upper respiratory infection and blood-
stained tears upon crying vigorously which subsided
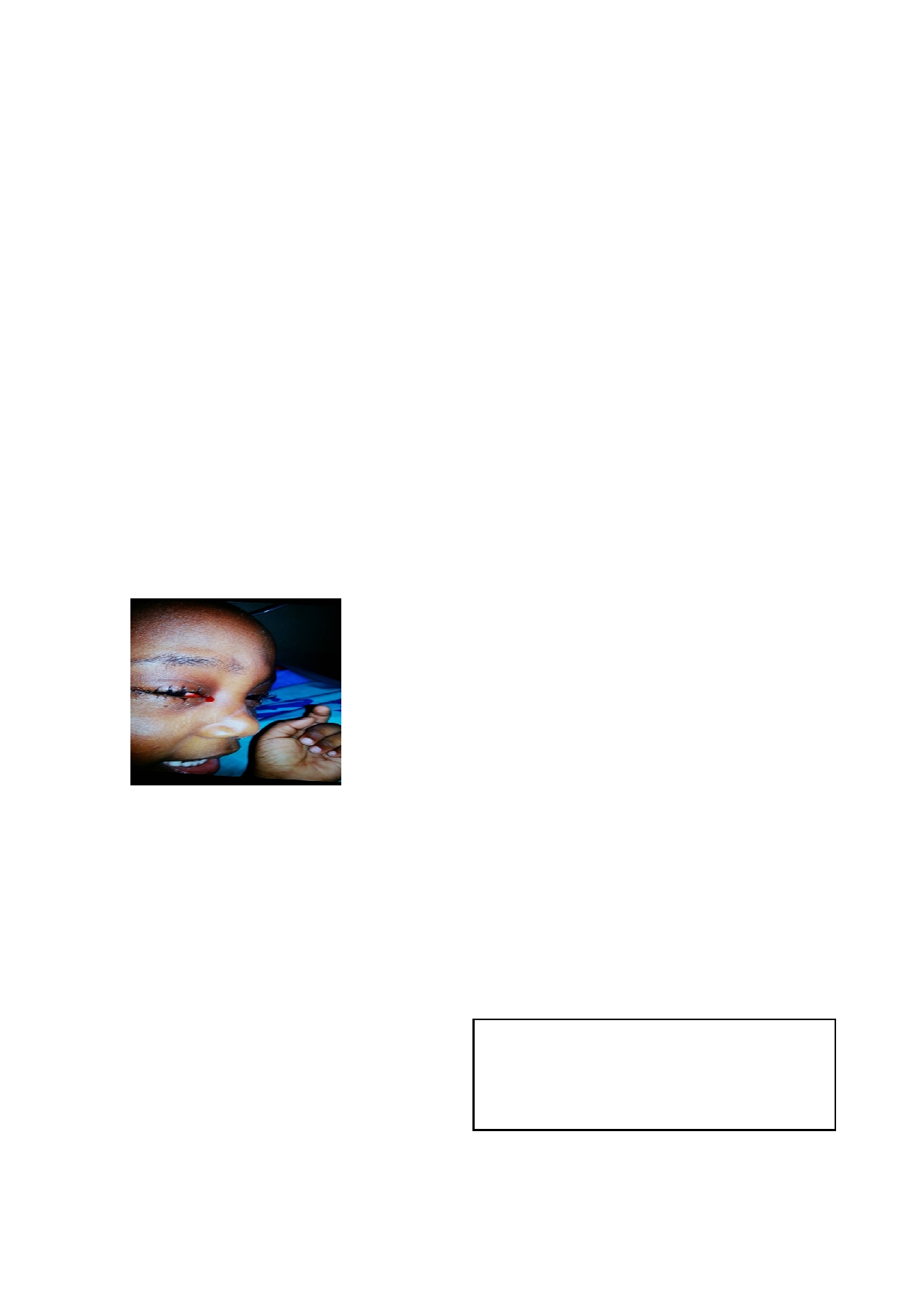
SA, a four year old female, presented in the above pri-
simultaneously with the clearing of the infection. A
vate hospital (about a year after Case 1) with redness of
similar scenario was seen in our second patient whose
the eyes and yellowish mucoid discharge of six days,
bloody tearing resolved with recovery from the infective
low-grade fever of three days and spontaneous bloody
episode.
tears from both eyes. There was associated gradual pain-
Ho
et al also documented spontaneous bloody tearing in
2
ful swelling of the eyes which occluded the right eye
and also impaired her vision. There was associated pro-
a
case series comprising a six-year old boy and three
jectile vomiting, which was neither blood-stained nor
girls ( two aged 12 years and one 14 years) over an 11-
bilious but contained recently ingested feeds. There was
year period. These patients had extensive work which
no
bleeding from any other body orifice. However there
failed to suggest a cause. The bloody tearing eventually
was a history of frequent uncontrollable flow of tears
resolved in all these patients without further sequel nor
without any emotional involvement since birth. On ex-
recurrence over a follow-up period of 9 months to 11
years .
2
amination,
she
was
acutely
ill
looking,
febrile
(temperature of 38.2°C) and had bilateral hyperaemic
swollen eyes with yellowish discharge and intermittent
Evaluation and management of haemolacria is multidis-
shedding of bloody tears. Full blood count was sugges-
ciplinary. A thorough history, a careful eye examination
and
an otolaryngologic examination are essential . Ex-
3
tive
of sepsis. Coagulation profile and eye swab micros-
copy
were normal while culture yielded no growth. She
tensive workup is also required to establish a diagnosis.
was
commenced on intravenous antibiotics (Augmentin
When
one is suspicious about the nature of the red mate-
and
Gentamicin) and chloramphenicol eye drops. Fac-
rial
such as suspected hysteria and malingering, micros-
tors
VIII and IX assays were normal. CT scan of both
copy
and tests to detect and analyze blood are worth-
while .
8
eyes
and lacrimal gland biopsy were planned after re-
view
by the ophthalmologist though not eventually done
due
to financial constraints. The child improved with
Treatment is guided by the aetiology. These may include
resolution of symptoms. She is being followed up and
administration of antibiotics, correction of a bleeding
has
not had any bloody tears for six months.
diathesis, tumor removal, hormonal therapy, antituber-
culous drugs, anti-thyroid medications or psychother-
apy
3-5,7-9
.
High dose vitamin C has been postulated to be
effective in bloody tearing caused by chronic inflamma-
tory
conditions . In our first patient, it is not easy to at-
6
tribute resolution of haemolacria entirely to Vitamin C
therapy. Close observation with reassurance is needed in
idiopathic cases as most will resolve spontaneously.
Counseling and psychological support for patients and
family is useful in helping the family to cope with possi-
ble
discrimination and stigmatization especially in
superstitious settings.
Discussion
Conclusion
Different isolated cases of haemolacria are reported in
In
conclusion, haemolacria is an uncommon but worri-
literature. All age groups can be affected from infancy to
some clinical phenomenon. Management involves a
the elderly which would as expected be related to the
multidisciplinary approach. Financial constraints may
causative factors. There is no obvious sex preponder-
constitute a challenge in full evaluation and management
ance except where the primary disease has a gender bias
in
resource-constrained settings. Follow up of patients is
such as hyperthyroidism or hysteria . Coincidentally,
7
8
recommended.
our
patients were both four years old at presentation but
a
male and a female respectively.
Authors Contributors
Some reports have documented haemolacria accompa-
OEE : managed the first case
nying epistaxis as was seen initially in our first patient.
3,4
ACH
: managed the second case. Both authors wrote
The anatomical basis of this occurrence lies in the inti-
and reviewed the manuscript.
mate connection of nose and eye via the lacrimal appara-
Conflict of interest: None
tus . An increase in pressure within the nasal cavity dur-
4
Funding: None
ing epistaxis can cause retrograde flow of blood through
the system and thus lead to bloody tears emerging from
the ipsilateral eye . Other reports of bloody tears in early
4
childhood include Scott, who described a 6-month-old
2

70
Acknowledgements
We
also appreciate the Management of Motayo Hospital
Limited for permission to use their patients’
The
authors wish to thank the parents of the patients for
information.
their consent to use the information and photographs.
References
1.
Dodonaeus R. De Lachrymis san-
4.
Scott ZR. Sanguineous lacrimation
7.
Ho
JZS, de Silva J, Olver J. A
guineis. In: Medicinalium Obser-
AMA J Dis Child 1927; 33: 907-9.
very rare case of bloody tears with
vationum exempla rara, Coloniae.
5.
Awan S, Kazmi HS, Awan AS.An
enigmatic epistaxis and haema-
1581.
unusual case of bloody tears. J
turia. Orbit
2011; 30:116-7.
2.
Ho
VH, Wilson MV, Linder JS,
Ayub Med Coll Abbottabad
8.
Ahluwalia BK, Khurana AK, Sood
Fleming JC, Haik BG. Bloody
2006;18:68-9.
S.
Bloody tears (haemolacria).
tears of unknown cause: case se-
6.
Karslioglu S, Ş im ş ek IB, Akbaba
Indian J Ophthalmol 1987;35:41-
ries and review of the literature.
M.
A case of recurrent bloody
3.
Ophthal Plast Reconstr Surg
tears. Clinical
Ophthalmology
9.
Jablenska L, Lo S, Uddin J, Toma
2004; 20(6): 442-7.
2011:5 1067–9.
A.Nasolacrimal tuberculosis: case
3.
Wiese MF .Bloody tears, and
report highlighting the need for
more! An unusual case of epis-
imaging in identifying and manag-
taxis. Br
J Ophthalmol
2003;
ing
it effectively. Orbit
87:1051.
2010;29:126-8.